by Kayla Bachand, MSN, AGNP-C

Constipation, the inability to pass your body’s waste through a bowel movement, is a common occurrence for many adults. There are two types of constipation: occasional and chronic. Occasional constipation means having less than three bowel movements a week, while chronic constipation is described as frequent, persistent difficulty passing bowel movements for an extended period.
According to the American Gastroenterological Association, constipation affects approximately 16 percent of adults and 33 percent of adults older than 60 years of age. As we age and our bodies and habits change, constipation can become more frequent and lead to more concerning medical issues.
Common causes of constipation include decreased water intake, changes in diet, medication, lack of physical exercise and more.
Constipation by itself is not typically life-threatening, but it can become more serious when a person has one or more underlying health conditions. This is especially true for the older population.
5 Ways to Help Ease & Prevent Constipation
1. Adequate Water Intake. The average person doesn’t consume enough water, which causes dehydration and makes you more prone to constipation. It’s recommended you drink half of your body weight in ounces of water, unless you have a medical condition that advises against it. For example, someone who weighs 200 pounds should drink at least 100 ounces of water per day. When you start consuming the recommended ounces, you will need to use the bathroom more often, but eventually your body will adjust to the extra water intake. Unfortunately, no other liquids can replace water—not even coffee, energy drinks or soda.
TIP: Try using a large glass or water bottle with the ounces clearly visible on the vessel. This will help you track how many refills you need to drink to reach your goal.
2. Physical Activity. Moving your body helps get your bowels moving, too. Movement as simple as a stroll around your house or apartment can impact the function of your digestive tract.
3. Fiber Intake. The recommended daily fiber intake is 20-25 grams. Fiber can be found in the form of whole grain breads, unrefined cereals, flax meal or bran, vegetables and fruit. Make sure you are drinking enough water while consuming fiber. (Examples of 20-25 grams of fiber: 2.5 cups of raspberries, blackberries or blueberries; four medium pears or apples; three large bananas; one cup of Fiber One cereal by General Mills or All-Bran or Raisin Bran by Kellogg’s; beans provide lots of fiber, 1.5 cups of lima or pinto beans)
TIP: Try to increase your fiber intake slowly over a two to three-week period. An increase in too much fiber too quickly can lead to abdominal bloating or gas.
4. Abdominal Massage. Gentle abdominal massage can encourage bowel movement if done properly. Use the “I Love U” technique in three passes.
- I – It’s important to start in the lower right side of your stomach and gently massage your stomach with one or two hands making small circles and slowly moving up the right side. This is the “I.”
- Love – Then stop, and start over again, but this time continue across the upper portion of your stomach, below your rib cage. This is the “L” in love.
- U – Then stop, and start over, this time you will continue down the left side and then stop. This is the “U” pass.
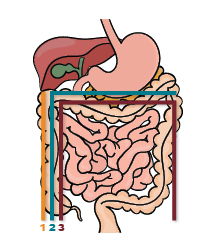
‘I Love U’ Abdominal Massage
TIP: Always remember to start bottom right and move right to left; use the diagram to the left as a guide. You can perform this technique as often as you want. It can also help facilitate movement when having gas pains.
5. Medications. There are several different medications that can help with constipation. You should always discuss medications with your medical provider before starting new medications; this includes over-the-counter medication. Although medication can assist in relieving constipation, it’s recommended to only use them after other techniques have failed because of the side effects that come along with any medication. Medications used to help with constipation include bulking agents, osmotic laxatives, stimulant laxatives and stool softeners.
- Bulking laxatives: These add bulk to the stool by absorbing water into the gut, which makes the stool soft and easier to pass. The most common is psyllium (Metamucil). This should be taken with plenty of water to avoid a bowel obstruction.
- Osmotic laxatives: These soften and ease stool by gently attracting water into the colon. Magnesium hydroxide (Milk of Magnesia), polyethylene glycol (MiraLAX) and lactulose are examples of this type of laxative.
- Stimulant laxatives: These work by causing the intestinal muscles to contract and push out, or “stimulate” a bowel movement. Sennosides (Senna) and bisacodyl (Dulcolax) are two types of stimulant laxatives.
- Stool softeners: Stool softeners are blended into the stool mass and provide lubrication for easier passage of the stool. Docusate sodium is an example of a stool softener.
Simple adjustments to your daily routine can help prevent constipation and are the most effective way to treat it. Incorporate the tips 1-3 from above into your daily habits with support from tips 4-5, and you should see improvement in your personal comfort as well as your bowel movements.
If you or your loved one lives with a chronic illness, House Calls may be able to help. House Calls brings primary care to your front door for individuals who have difficulty leaving their homes for routine medical appointments. Contact us today to learn more.
Kayla Bachand is a certified adult-gerontology nurse practitioner with House Calls.



